What is Depression?
Today, it seems like every other person you talk to is anxious or depressed. And you wouldn’t be far wrong. Depression now affects approximately 1 in 4 women and 1 in 10 men of working age.
In fact, depression is now thought to be the second leading cause of disability worldwide.
In this article I am going to explain what depression is, explore the theories behind it and provide strategies that may help address the roots of depression.
What is Depression?
Clinical depression or major depressive disorder (MDD) is a mood disorder that presents with unremitting sadness, sleep disturbance, brain fog, loss of appetite, fatigue and diminished interest in pleasure (anhedonia) (NICE, 2015).
For those of us who don’t live in a textbook: what does that really mean? Like many illnesses there exists a spectrum.
At the light end people can feel overwhelmingly sad and hopeless and their senses can often feel ‘blunted’. They can function but feel like they are merely existing.
At the darker end, people can feel like they’ve been consumed by a black hole. These people experience the deepest and darkest depths of despair, hopelessness and defeat. These people can calmly and plainly rationalize their non-existence. It is a very uncanny experience, where internally you sit in peaceful acceptance of the possibility of non-existence. Even stranger, you function ‘normally’ and everything appears normal from the outside. It’s a truly bizarre experience as if you are almost in a trance (like coming into contact with a ‘dementor’).
Coming back to the ‘textbooks’ or ‘manuals’ as dear Donald Trump once described in his interview with Axios: Depression is normally diagnosed using the criteria from the International Classification of Diseases (ICD-10) or Diagnostic and Statistical Manual of Mental Disorders (DSM-5) for those in the U.S.
The criteria state you must have five or more symptoms in a two-week period with at least one from the first two listed:
- Depressed mood reported by self and observed by others
- Loss of interest in pleasure (anhedonia)
- Fatigue
- Poor concentration or indecisiveness
- Insomnia or hypersomnia (sleepy all the time)
- Loss of appetite
- Suicidal thoughts
- Physical agitation or retardation (not moving much)
- Reduced libido
Please note: depression exists in many forms including seasonal, psychotic, perinatal, manic and persistent depression. This article is focusing on the ‘mainstream’ flavour known as major depressive disorder. As the symptoms of depression can mimic other conditions it’s important to speak to your GP or internist.
Theories of Depression
Unfortunately, the precise causes of depression remain unclear. However, researchers, believe it is a multifactorial condition involving our biology, psychology and environment.
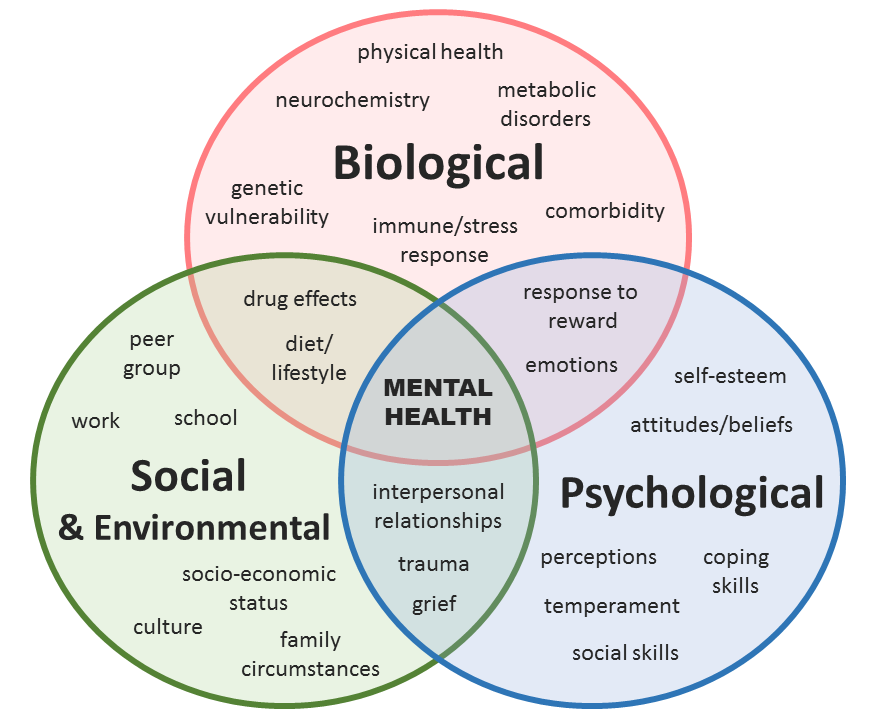
Risk factors include patients with a family history of depression, suicide attempts or victims of abuse, coronary heart disease, pain syndromes, thyroid disease, schizophrenia, dementia, Parkinson’s, multiple sclerosis and stroke. It’s also important to know that depression often accompanies other ‘mental disorders’ including anxiety or GAD and bipolar disorder.
But what about anti-depressants? What do they do?
Antidepressants are predicated on the ‘monoamine hypothesis’ which suggests depressed people have a deficiency in synaptic (brain) concentrations of norepinerpherine, dopamine and serotonin.
For a detailed history of how this theory was devised I recommend reading ‘the chemical imbalance myth’ by Chris Kresser.
Here is a brief summary: In the 1950’s resperine a compound isolated from the plant Rauwolfia Serpentina was found to decrease norepinephrine, dopamine and serotonin in animal studies. When resperine was administered to these animals, they developed hunched posture and immobility (arguably a sign of depression). Therefore, low dopamine, serotoin and norepinephrine (monoamines) in the brain was believed to be the cause of depression.
I won’t be diving into the ‘nitty gritty’ of this singular theory. All I will say is, surprisingly there is not yet a single peer-reviewed piece of research that shows any mental disorder occurs as a result of low serotonin.
Furthermore, the DSM or ICD-10 (the manual used by American psychiatrists) does not list serotonin as a cause of any mental disorder. It is also well-known that it takes a couple weeks to experience any noticeable change in mood, yet we know antidepressants can increase amine levels in one or two days.
But you maybe thinking, but antidepressants have helped me. They must be doing something?
As I don’t want this article to be too long, I will explore this question in another post, but if you remember one thing from this article:
Like many conditions, they are complex and nuanced and there are many moving parts. To maximize your chances of success we must do our best to address as many as we can. What we describe as depression, is likely a consequence of a number of physical issues. Antidepressant may work for a few of them in a subset of patients.
In my practice, I rarely see someone who is seeing me exclusively for their depression symptoms. Often, their depression accompanies gut issues, overweight and autoimmune conditions. What do all these conditions share in common?
Inflammation.
The cytokine model of depression
Researchers are beginning to uncover the relationship between our brains and our immune system, giving birth to a field called neuro-immunology. An important player in this relationship is the gut-brain axis.
The gut-brain axis is a bidirectional model linking our emotional and cognitive functions with gastrointestinal functions. In other words, we are beginning to understand the impacts of our thoughts and emotions on the health of our guts and vice versa.
It has been suggested the onset of depression is caused by chronic emotional and physical stressors such as stress, poor sleep, junk food diets, smoking and alcohol. This is possibly linked to immune activation and neuroendocrine dysregulation potentially driven by our guts.
Depression is believed to occur when the Hypothalamic-Pituitary-Adrenal system is chronically activated causing a hypersecretion of corticotrophin-releasing hormone (CRH) leading to chronic elevations of cortisol resulting in immune dysregulation i.e. unwanted inflammation.
In other words, chronic and persistent stress can ‘confuse’ our immune systems and cause inflammation.
Whenever our immune system has to work to protect us from injury or infection, immune cells gather to repair and heal. This happens when messenger molecules called cytokines are released by our white blood cells.
Scientists began to observe when compared to non-depressed individuals, people with MDD had elevated levels of inflammatory markers and cytokines (including ESR, TNF-α, IL1- α and IL-6 and COX-1 and COX-2 if you’re interested). These were found in both medically fit and medically unfit patients.
At this stage, these findings are merely observational, and what I am about to describe has been discovered using mice and observed in brain’s of severely depressed people:
So here is how it potentially works:
Increased intestinal permeability aka ‘leaky gut’ is believed to cause bacterial and macromolecule translocation across the gut wall into circulation.
‘Bits’ belonging to the wall of these molecules known as Pathogen-associated molecular patterns (PAMPI’s) or lipopolysaccharides (LPS) bind to receptors on macrophages (white blood cells) signaling to the immune system something is wrong. As a result, NF-kB (a chemical that switches inflammatory genes on) and various cytokines are produced circulating the body.
Two things then happen:
- The circulating cytokines bind to ‘cytokine-specific transport molecules’ on the blood brain barrier and enter the brain to signal inflammation.
- The cytokines activate the vagus nerve to transmit inflammatory signals to brain nuclei in the hypothalamus, hippocampus, amygdala and prefrontal cortex causing activation of the brain’s immune cells called microglia.
As microglia become inflamed, the amino acid tryptophan which is normally converted to serotonin (remember this guy) is instead converted to kynurenine and quinolinic acid. This is not good, because in high amounts, they can overstimulate our glutamate (NMDA) receptors, which promotes neuronal cell death and oxidative stress and consequently affects neuro-circuitry manifesting in behavioral and cognitive deficits observed in depression.
As neat as this theory sounds, it must be emphasized that although a multitude of studies have demonstrated increased levels of inflammatory markers, there is still considerable variability within depressed populations.
It is believed that inflammation is associated with depression in a subtype of patients with genetic and biological predispositions.
One day anti-inflammatory drugs or those with similar actions maybe prescribed for people with an ‘inflammatory type’ of depression.
So what does this mean for me? How can I help my depression?
The good news is, although mainstream medicine is far away from developing personalized drug therapies, there is a lot that can be done outside of the doctor’s office.
In fact, popular to contrary belief antidepressants are not used as a first-line treatment for mild to moderate depression. Instead, low-intensity psychological interventions including guided self-help, cognitive behavioral therapy and counselling are recommended.
Diet
Studies have observed a possible link between poor diet quality and increased depression risk. Diets high in alcohol and refined carbohydrate intake and diets low in B vitamins, magnesium, vitamin D, omega fatty acids have been associated with increased rates of depression.
Conversely, a Mediterranean style diet, with a focus on high intakes of fruit, vegetable, fish and low intakes of refined foods, may play a protective role. We are beginning to understand that a nutrient dense diet can help reduce oxidative stress, inflammation and mitochondrial dysfunction. So eating a whole foods diet may help address inflammation related depression by removing potential drivers and boosting nutrient status.
What does this mean in English?
Aiming for at least 5 (ideally 8) portions of green leafy/cruciferous and starchy vegetables per day. Reducing and cutting out refined or processed foods and reducing alcohol.
I must emphasize that by embracing a nutrient dense diet you are dramatically improving all aspects of your health.
Mindfulness based practice
Mindfulness practice has been shown to reduce stress hormones and purported to reduce inflammatory cytokine levels. Studies have found that 20 minutes twice per day can improve self-reported mood and stress tolerance.
There are a multitude of apps and programs that can help you do this. I’ve written an article on how to integrate meditation into your daily routine. I personally enjoy Dr Lawrence Wilson’s pushing down exercise.
Exercise
Several studies have shown aerobic exercise to be as effective as SSRI’s when engaging in moderate exercise five times per week and can lead to remission.
In practice, this may look like 30 minutes per day up to five times per week engaging in exercise you enjoy. Riding your bike, running, sport or even yoga.
Personally, I don’t believe exercise is a long-term remedy but more of a palliative remedy. Exercise has a multitude of benefits, so there is nothing to lose while you are addressing the root cause.
Curcumin
Although, there are supplements with more complete evidence such as St John’s Wort.
In my experience, if there was a single remedy or intervention I could recommend to somebody with depression it would be curcumin.
And I’m not talking about adding a teaspoon to your tea in the morning. I’m talking about a formula designed to maximize uptake and synergistically address the target.
Up until recently that was a formula called KappaRest from Biotics Research, however, based on my latest findings I’ve moved on to their latest formula called curcumRx.
CurcumRx is special because the turmeric root has been emulsified, concentrating as many as 200 nutrients and greatly enhancing bioavailability. Interestingly, turmeric helps inhibit NF-kB reducing the inflammatory mediators.
There is evidence from several large scale studies (meta-analyses) that suggest it can have an effect on depressive and anxiety symptoms. These are, however, still small sample sizes and more research will be needed to prove it’s effectiveness for the mainstream crowds.
Getting to the root
There are multiple therapies and techniques that have been studied which I have not mentioned such as psychotherapy, cognitive behavioural therapy, light therapy, acupuncture and sleep hygiene.
The important thing to remember is that health is a team sport and like many conditions depression is most likely caused by a number of different things.
Remember the roads between our brain and body are two way streets and making our bodies stronger has the potential to change the way our brains process and interpret our thoughts, feelings and emotions.

It’s our bodies imperative to survive and thrive and our natural state is to be happy and productive.
Asking yourself why some people are able to thrive in the face of trauma and adversity while others suffer for many years, I hope can serve as some inspiration if you are struggling with mental health.
To maximise your chances to thrive I recommend addressing as many ‘moving parts’ as possible.
Wishing you well on your path to health,
Inder


0 Comments